‘A complete shift’: Not just ventilators, doctors now use a range of COVID-19 treatments

Dramatic drop in patients on ventilation shows impact of new methods
By Lilo H. Stainton, NJSpotlight
When the first wave of coronavirus patients flooded New Jersey hospitals earlier this year, clinicians were heavily focused on ventilators. At the apex of the pandemic, one in four people hospitalized for COVID-19 needed these machines to breathe, and the state’s supplies were running short.
Six months later, the picture has changed dramatically. Ventilators are still critical for some patients — 10% of those hospitalized earlier this week depended on artificial respiration, according to state data — but clinicians now try to employ less invasive protocols first, like high-flow oxygen or repositioning patients to ease breathing, called “proning.”
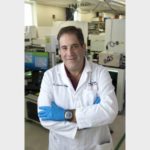
“When the pandemic started, we intubated you at the drop of a hat,” said Dr. Lewis Nelson, who leads the emergency department at University Hospital in Newark, which was at the heart of the outbreak. Intubation generally requires the patient to be heavily sedated as a tube is then inserted into the windpipe and connected to the ventilator, which is calibrated to provide a specific oxygen concentration. The patient often requires a catheter to collect urine as well.